
Why Bone Grafts Matter for Dental Implants
Dental implants have revolutionized modern dentistry by offering a reliable, long-term solution for missing teeth. However, not every patient is immediately eligible for implants — especially if there has been significant bone loss in the jaw due to tooth extraction, gum disease, or long-term edentulism.
This is where bone grafting comes into play: an advanced surgical technique that rebuilds lost bone structure, creating a stable foundation for dental implants to integrate successfully.
In Turkey, innovative bone grafting techniques — used in conjunction with dental implant surgery — ensure that even patients with severe jawbone loss can receive long-lasting, natural-looking results.
What Is Bone Grafting for Dental Implants?
Bone grafting for dental implants is an advanced surgical procedure designed to restore or preserve jawbone volume in areas where natural bone has been lost or is insufficient to support implant placement. Dental implants rely on a strong and dense bone foundation to remain stable over time; without adequate bone quantity and quality, implant success may be compromised.
When a natural tooth is present, its root continuously stimulates the surrounding jawbone during chewing and biting. Once a tooth is lost or extracted, this stimulation ceases, triggering a biological process known as bone resorption, in which the body gradually breaks down and absorbs the unused bone. Over time, this leads to reduced bone height, width, and density — all of which are critical factors for successful implant anchorage.
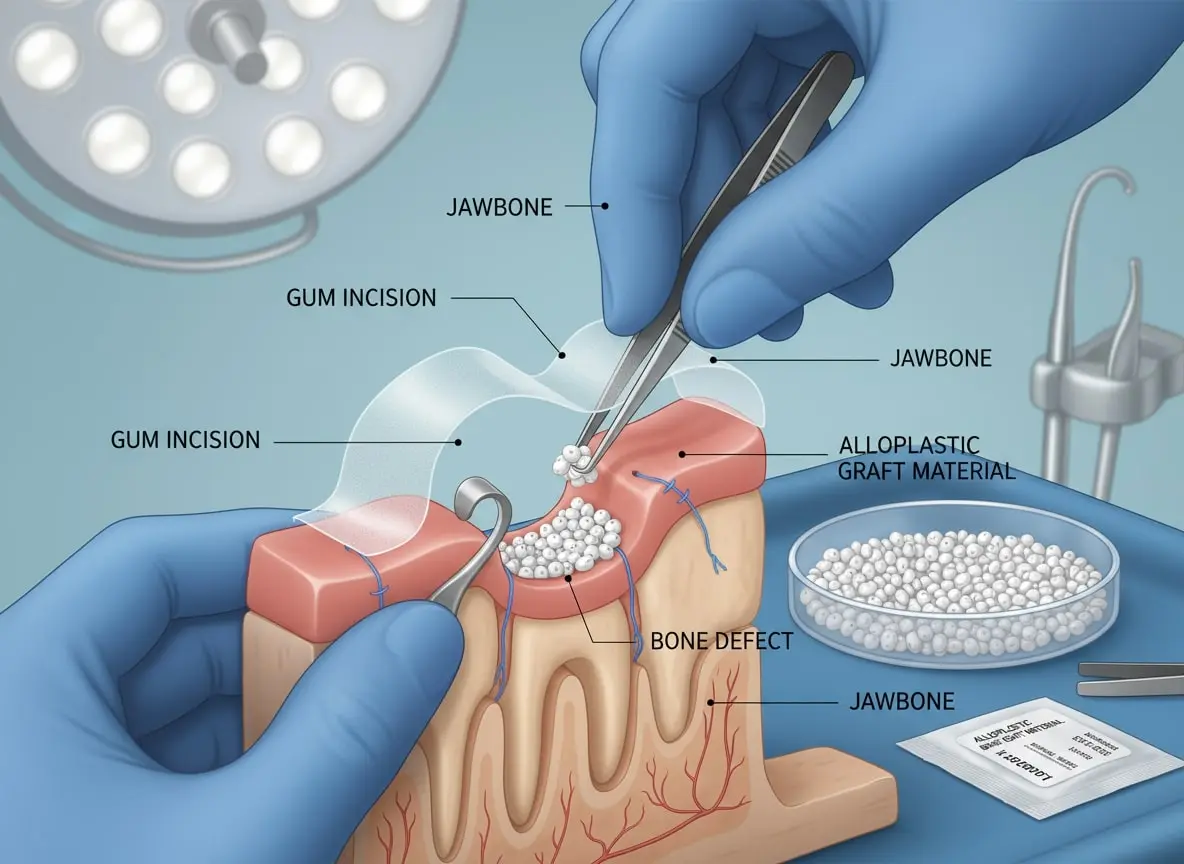
Bone grafting works by introducing biocompatible graft material into the deficient area of the jaw. This material acts as a scaffold, encouraging the patient’s own bone cells to migrate, regenerate, and form new, living bone. As healing progresses, the graft material is partially or fully replaced by the patient’s natural bone through a process called osseous remodeling.
In implant dentistry, bone grafting is not merely a preparatory step — it is a biological reconstruction process that restores the jaw to a condition capable of long-term implant stability, function, and aesthetics.
Why Bone Grafting Is Critical for Implant Success
Dental implants are designed to fuse directly with the jawbone through a process called osseointegration. This fusion requires:
- Adequate bone volume (height and width)
- Sufficient bone density
- Proper vascularization (blood supply)
If any of these conditions are lacking, the implant may fail to integrate properly, leading to:
- Implant mobility
- Bone loss around the implant
- Inflammation or peri-implantitis
- Eventual implant failure
Bone grafting addresses these risks by re-establishing ideal anatomical conditions before or during implant placement.
The Three Primary Goals of Bone Grafting in Implant Dentistry
1. Rebuilding Lost Bone Volume
Bone grafting restores jawbone that has deteriorated due to:
- Long-term tooth loss
- Periodontal (gum) disease
- Trauma or infection
- Poorly fitting dentures
By increasing bone height and width, grafting allows implants to be placed in the correct anatomical position, improving both mechanical stability and aesthetic outcomes.
2. Preserving Bone After Tooth Extraction (Socket Preservation)
Socket preservation is a specialized form of bone grafting performed immediately after tooth extraction. Without intervention, the extraction socket can lose up to 50% of its bone volume within the first year, with the most rapid loss occurring in the first 3–6 months.
By placing graft material directly into the empty socket:
- Bone collapse is minimized
- Natural jaw contours are maintained
- Future implant placement becomes easier and more predictable
This technique is especially important in the front (aesthetic) zone, where bone loss can negatively affect gum contours and smile symmetry.
3. Creating a Stable Foundation for Dental Implants
Ultimately, bone grafting ensures that dental implants can be:
- Securely anchored
- Properly aligned
- Evenly loaded during chewing
A well-integrated graft creates a biologically and mechanically stable base, allowing the implant to withstand long-term functional forces without compromising surrounding bone or soft tissue.
In many cases, bone grafting also enables:
- Immediate or early implant placement
- Reduced risk of implant failure
- Improved long-term success rates
Why Bone Loss Happens After Tooth Extraction
When a natural tooth is lost or extracted, the effects go far beyond the visible gap in the smile. Beneath the surface, the jawbone immediately begins to change. This process, known medically as bone resorption, is a natural biological response in which the body gradually breaks down and absorbs bone tissue that is no longer being stimulated.
The Role of Tooth Roots in Bone Health
Healthy teeth play a critical role in maintaining jawbone density. Every time you chew or bite, the tooth roots transmit pressure to the surrounding bone. This mechanical stimulation signals the body to continuously remodel and preserve the bone structure.
Once a tooth is removed:
- The root is no longer present
- The bone stops receiving stimulation
- Blood supply to the area decreases
- The body interprets the bone as “unnecessary”
- Gradual bone shrinkage begins
This process can start within weeks after extraction and continue progressively over months and years if no restorative treatment (such as implants or grafting) is performed.
Jawbone Resorption: A Progressive Process
Bone resorption does not occur all at once. Instead, it happens in stages:
- Early Phase (First 3–6 Months)
- Rapid loss of bone height and width
- Most noticeable volume reduction
- Implant placement may already become more challenging
- Mid-Term Phase (6–12 Months)
- Continued bone thinning
- Changes in gum contour
- Increased aesthetic and functional compromise
- Long-Term Phase (1+ Years)
- Significant loss of jawbone volume
- Facial sagging or premature aging appearance
- Severe limitations for implant placement without grafting
Studies show that up to 25% of bone width can be lost in the first year after tooth extraction if no intervention is performed.
Common Causes of Significant Bone Loss
While tooth extraction is a major trigger, several conditions accelerate or worsen bone loss:
- Long-term missing teeth
Empty spaces left untreated for years lead to severe bone collapse. - Advanced periodontal (gum) disease
Chronic infection destroys both gum tissue and supporting bone. - Dental trauma or injury
Accidents can damage bone even if the tooth is later removed. - Untreated infection or abscess
Inflammation and bacteria erode bone tissue over time. - Congenital or developmental bone deficiencies
Some patients naturally have insufficient jawbone volume. - Long-term removable denture wear
Dentures rest on the gums and accelerate bone resorption due to pressure and lack of stimulation.
Impact of Bone Loss on Oral and Facial Health
Untreated jawbone loss affects far more than implant eligibility:
- ❌ Difficulty chewing and speaking
- ❌ Poor denture stability
- ❌ Shifting of neighboring teeth
- ❌ Bite misalignment (malocclusion)
- ❌ Sunken facial appearance
- ❌ Premature aging around the mouth and jawline
From both a functional and aesthetic perspective, preserving or rebuilding bone is essential for long-term oral health.

Types of Bone Grafts in Implant Dentistry
Dental professionals use several types of bone graft materials, depending on the patient’s individual needs and clinical condition:
1. Autograft (Patient’s Own Bone)
Bone harvested from the patient’s own body — usually from the chin, jaw, or hip — is considered the gold standard because it contains living cells and growth factors that promote rapid bone regeneration.
Pros:
✔ Highest integration rate
✔ Low risk of immune rejection
Cons:
⚠ Requires additional surgical site
⚠ Slightly higher surgical time and recovery
2. Allograft (Human Donor Bone)
Bone obtained from a human donor (tissue bank) that has been processed and sterilized.
Pros:
✔ Excellent bone-building potential
✔ No second surgical site required
✔ Commonly used in implant cases
Cons:
⚠ Slightly slower integration than autografts (but still highly effective)
3. Xenograft (Animal-Derived Bone)
Typically sourced from bovine (cow) bone, xenografts provide a scaffold for the patient’s own bone to grow into.
Pros:
✔ Reliable and widely used
✔ Helps maintain bone volume
Cons:
⚠ No living cells — slower regenerative process
4. Alloplast (Synthetic Bone Graft)
Biocompatible synthetic substitutes (e.g., hydroxyapatite or tricalcium phosphate) that mimic natural bone.
Pros:
✔ No biological disease transmission
✔ Predictable outcomes
Cons:
⚠ May take longer to integrate fully
When Is a Bone Graft Necessary Before Dental Implants?
Not every patient requires bone grafting prior to dental implant placement. However, adequate jawbone volume and density are essential for the long-term stability, safety, and success of dental implants. When the natural bone structure is compromised, bone grafting becomes a critical preparatory step.
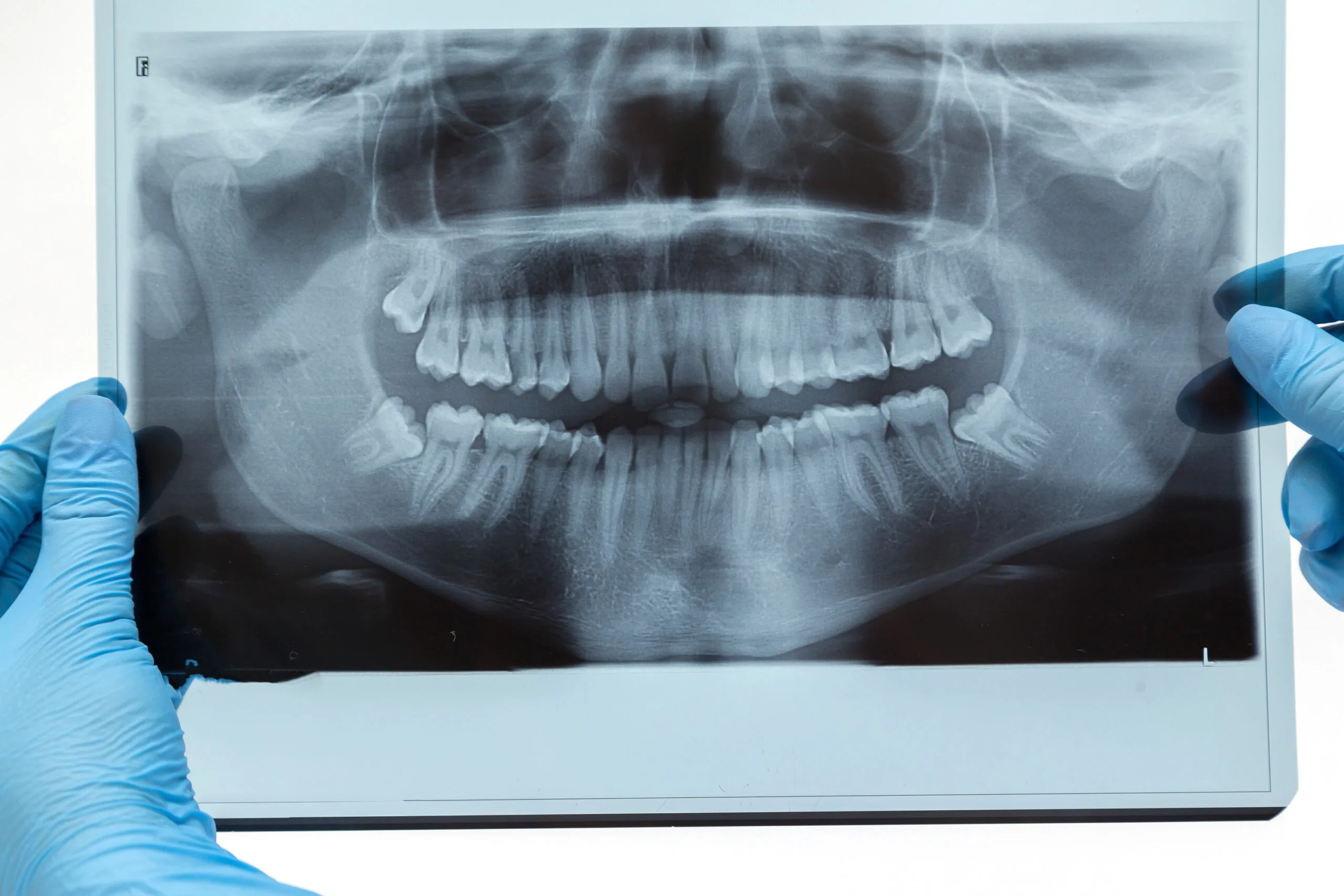
Your implant specialist may recommend a bone graft after a detailed clinical examination and 3D CBCT scan analysis, particularly in the following situations:
Insufficient Jawbone Width or Height
One of the most common reasons for bone grafting is insufficient bone volume in the implant site. This typically occurs when a tooth has been missing for an extended period.
After tooth loss:
- The jawbone no longer receives stimulation from chewing
- Bone begins to shrink (resorption)
- Both width and height of the bone decrease over time
If the bone is too thin or too short, it cannot securely anchor an implant. A bone graft restores the missing volume, creating a solid foundation for implant placement.
Common Misconceptions About Oral and Dental Health
.webp)
📌 All treatments and services will be carried out in health institutions accredited by the Turkish Ministry of Health and possessing a certificate of authorization in health tourism.
Advanced Bone Resorption Detected on CT Scans
Modern implant planning relies heavily on 3D cone beam computed tomography (CBCT). These scans allow specialists to precisely measure:
- Bone density
- Bone height
- Bone width
- Proximity to nerves and sinuses
If CT imaging reveals moderate to severe bone resorption, proceeding directly with implant placement may increase the risk of:
- Implant failure
- Poor osseointegration
- Long-term instability
In such cases, bone grafting is performed to rebuild lost bone tissue and optimize implant success rates.
Lack of Primary Implant Stability
For an implant to succeed, it must achieve primary stability—firm mechanical fixation in the bone at the time of placement.
Bone grafting is recommended when:
- The existing bone cannot securely hold the implant
- Immediate implant placement is not possible
- The risk of micromovement during healing is high
Without adequate stability, implants may fail to integrate with the bone (osseointegration), compromising the final outcome.
Sinus-Related Bone Deficiency (Sinus Lift Requirement)
In the upper posterior jaw, bone loss is often combined with sinus expansion. After tooth loss, the maxillary sinus gradually descends, reducing available bone height.
A sinus lift bone graft is required when:
- Bone height beneath the sinus is insufficient
- Standard implants cannot be safely placed
- Long-term implant stability is at risk
This advanced procedure gently elevates the sinus membrane and places graft material underneath, allowing new bone to form and enabling secure implant placement.
Long-Term Tooth Loss or Previous Implant Failure
Patients who have been missing teeth for many years or who experienced failed implants often present with significant bone loss. In these cases, bone grafting helps:
- Restore lost anatomical structure
- Improve future implant success
- Re-establish facial support and jaw strength
Why Bone Grafting Improves Implant Candidacy
Bone grafting is not a setback — it is a strategic investment in long-term oral health. By restoring proper bone volume, grafting:
- Expands implant eligibility for more patients
- Increases implant success rates significantly
- Enhances facial aesthetics and jaw stability
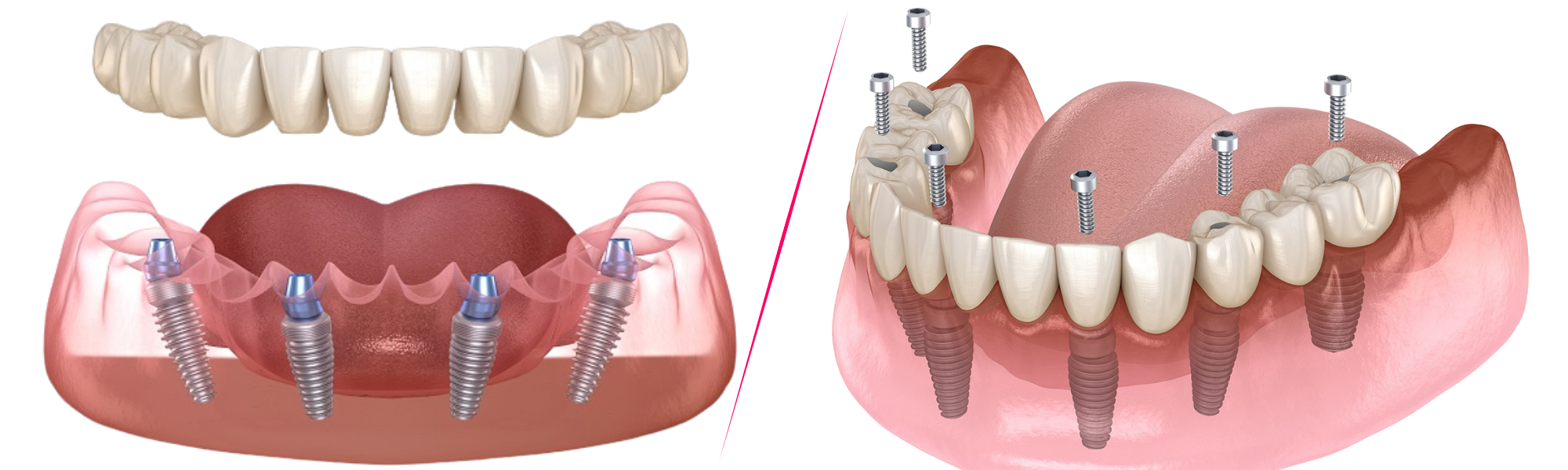
- Enables advanced solutions such as All-on-4 and All-on-6 systems
📌 Clinical Note:
All diagnostic imaging, bone grafting procedures, and implant treatments are performed in health institutions accredited by the Turkish Ministry of Health and authorized for health tourism, ensuring international safety and quality standards.
Bone Grafting Techniques Used in Turkey
Turkey has become a leader in advanced dental bone grafting due to precision surgical planning, cutting-edge technology, and high levels of clinical expertise.
1. Ridge Augmentation
Rebuilds horizontal bone loss in the jaw, creating width for implants.
2. Socket Preservation
Performed immediately after extraction to preserve bone volume.
3. Block Bone Grafts
Used in severe cases to rebuild large bone defects — especially in the front jaw region.
4. Sinus Lift (Maxillary Sinus Grafting)
Increases bone height in the upper jaw near the molars to allow implant placement.
How Bone Grafting and Implants Work Together
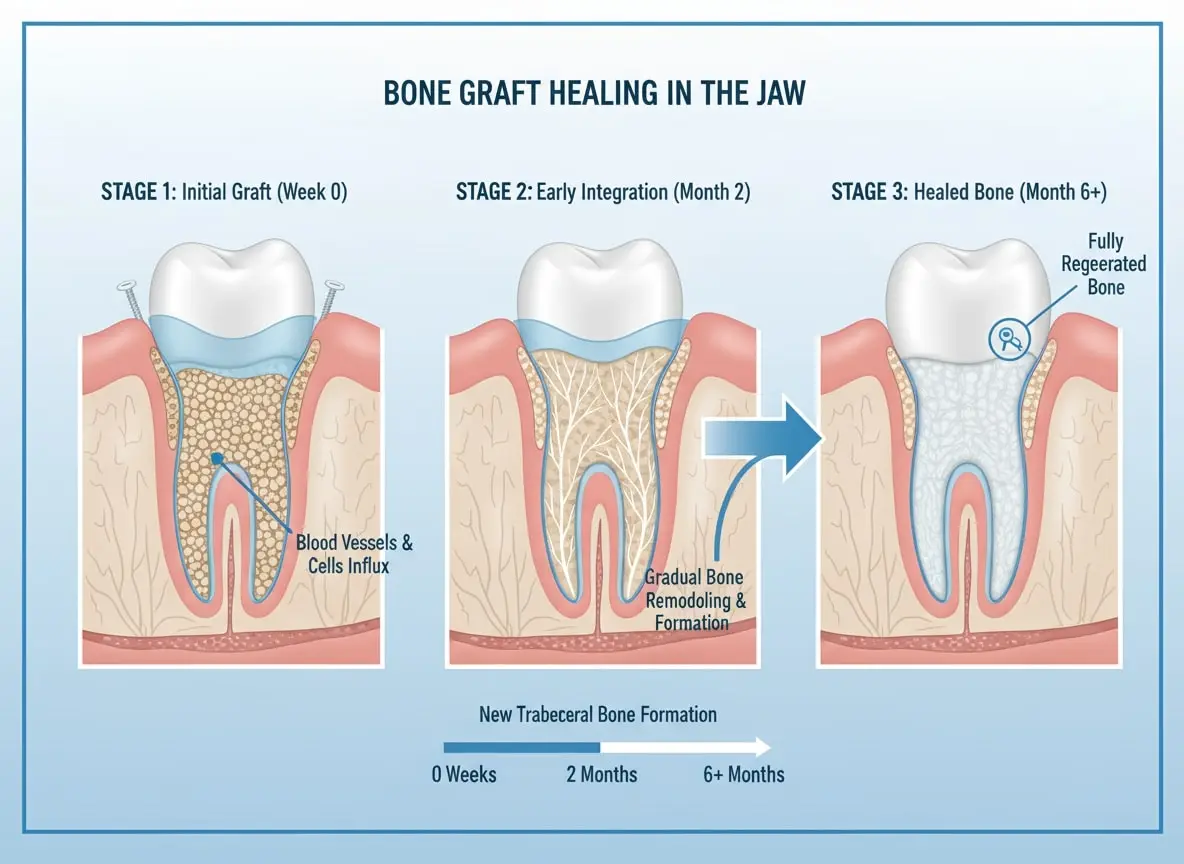
After bone graft placement, a healing period of 3–6 months is usually required for the graft to integrate and become strong enough to support implants.
Once sufficient bone volume is achieved:
- Dental implants are placed
- Osseointegration begins (implant fuses with bone)
- Final crowns, bridges, or dentures are attached
This collaborative process ensures high success rates and long-term stability.
Success Rates and Long-Term Outcomes
With modern techniques and proper planning, bone grafting in implant dentistry consistently shows success rates above 90%. Success depends on several factors:
✔ Quality of bone graft material
✔ Surgical expertise
✔ Patient health and lifestyle
✔ Good oral hygiene
In Turkey, many top clinics utilize digital planning, 3D imaging (CBCT), and guided surgical techniques, enhancing precision and outcomes.
Cost Overview: Bone Grafting in Turkey vs Other Countries

💡 Packages in Turkey often combine bone grafting + implant placement + crowns for a single transparent price.
Recovery and Aftercare
Typical Bone Graft Healing Timeline
- Days 1–3: Mild swelling, controlled with medication
- Week 1: Reduced discomfort
- Weeks 4–8: Gradual bone integration
- Months 3–6: Sufficient bone strength for implant placement
Good aftercare includes:
- Soft antibiotic mouth rinse
- No smoking
- Avoiding hard foods
- Follow-up visits and 3D scans
Risks and How They Are Minimized
Although bone grafting is generally very safe, potential risks include:
✔ Infection
✔ Graft failure or delayed integration
✔ Mild swelling or bruising
✔ Sinus complications (for sinus lift procedures)
In Turkey’s accredited clinics, these risks are minimized with:
- Strict sterilization protocols
- Digital surgical planning
- Experienced surgeons
- Personalized recovery plans
Frequently Asked Questions (FAQ)
1. Is bone grafting painful?
No — local anesthesia or sedation ensures comfort. Mild soreness afterward is normal.
2. How long before I can get implants after grafting?
Typically 3–6 months, depending on bone quality.
3. Can bone grafts fail?
Rarely, especially when placed by experienced surgeons and following aftercare.
4. Are grafts accepted in the body?
Yes — graft materials are biocompatible and integrate naturally.
5. Can sinus lift grafts be done simultaneously with implants?
In some cases, yes — if initial stability is achievable.
Bone Grafting — A Gateway to Lasting Dental Implants
Advanced bone grafting techniques have expanded the pool of candidates eligible for dental implants, especially those with significant jawbone loss. In Turkey — with its mix of clinical expertise, affordable care, and personalized patient experience — bone grafting is a powerful enabler for patients seeking a functional, durable, and beautiful smile.
📍 Ready to find out if bone grafting makes you a candidate for dental implants?
👉 Request a personalized consultation with our dental specialists
👉 Get a 3D CBCT evaluation before travelling
References
Albrektsson, T., & Johansson, C. (2001). Osteoinduction, osteoconduction and osseointegration. European Spine Journal, 10(S2), S96–S101.
Buser, D., Sennerby, L., & De Bruyn, H. (2017). Modern implant dentistry based on osseointegration: 50 years of progress, current trends, and open questions. Periodontology 2000, 73(1), 7–21.
Chiapasco, M., Casentini, P., & Zaniboni, M. (2009). Bone augmentation procedures in implant dentistry. International Journal of Oral & Maxillofacial Implants, 24(Suppl), 237–259.
Esposito, M., Grusovin, M. G., Felice, P., Karatzopoulos, G., Worthington, H. V., & Coulthard, P. (2009). Interventions for replacing missing teeth: Bone augmentation techniques for dental implant treatment. Cochrane Database of Systematic Reviews, (3), CD003607.
Jensen, O. T., & Terheyden, H. (2009). Bone augmentation procedures in localized defects in the alveolar ridge. International Journal of Oral & Maxillofacial Surgery, 38(Suppl 1), 218–236.
Misch, C. E. (2015). Dental Implant Prosthetics (2nd ed.). St. Louis, MO: Elsevier Mosby.
Misch, C. E., Suzuki, J. B., Misch-Dietsh, F. M., & Bidez, M. W. (2005). A positive correlation between occlusal trauma and peri-implant bone loss. Implant Dentistry, 14(2), 108–116.
Sanz, M., Dahlin, C., Apatzidou, D., Artzi, Z., Bozic, D., Calciolari, E., … Tomasi, C. (2019). Biomaterials and regenerative technologies used in bone regeneration in the oral cavity. Journal of Clinical Periodontology, 46(S21), 82–91.
Urban, I. A., Montero, E., Monje, A., & Sanz-Sánchez, I. (2019). Effectiveness of vertical ridge augmentation procedures. Journal of Clinical Periodontology, 46(S21), 291–306.
Wallace, S. S., & Froum, S. J. (2003). Effect of maxillary sinus augmentation on the survival of endosseous dental implants. Annals of Periodontology, 8(1), 328–343.
You May Like :
Root Canal Treatment: How to Save Your Tooth and Stop the Pain
Why Turkey Is #1 for Medical Tourism in 2025: Cost & Quality












.png)



.png)
.png)


.png)



